PHILADELPHIA — It’s not only tumors people battling cancer need to be concerned about. Researchers from the University of Pennsylvania School of Medicine have discovered that the liver could be a key reason why some cancers are hard to beat — and it’s all due to inflammation.
The findings, published in the journal Nature Immunology, shed light on why cancers that cause liver inflammation tend to have worse outcomes and respond poorly to cutting-edge treatments like immunotherapy.
The connection between liver inflammation and cancer comes down to proteins called serum amyloid A (SAA). UPenn researchers discovered that when cancer triggers inflammation in the liver, the organ’s cells start pumping out SAA proteins into the bloodstream, spelling trouble for the immune system’s cancer-fighting efforts.
“We want to better understand what causes cancer to resist or respond to immunotherapy to help design more effective strategies for patients,” says senior study author Dr. Gregory Beatty, an associate professor of Hematology-Oncology and the director of Clinical and Translational Research for the Penn Pancreatic Cancer Research Center, in a media release.

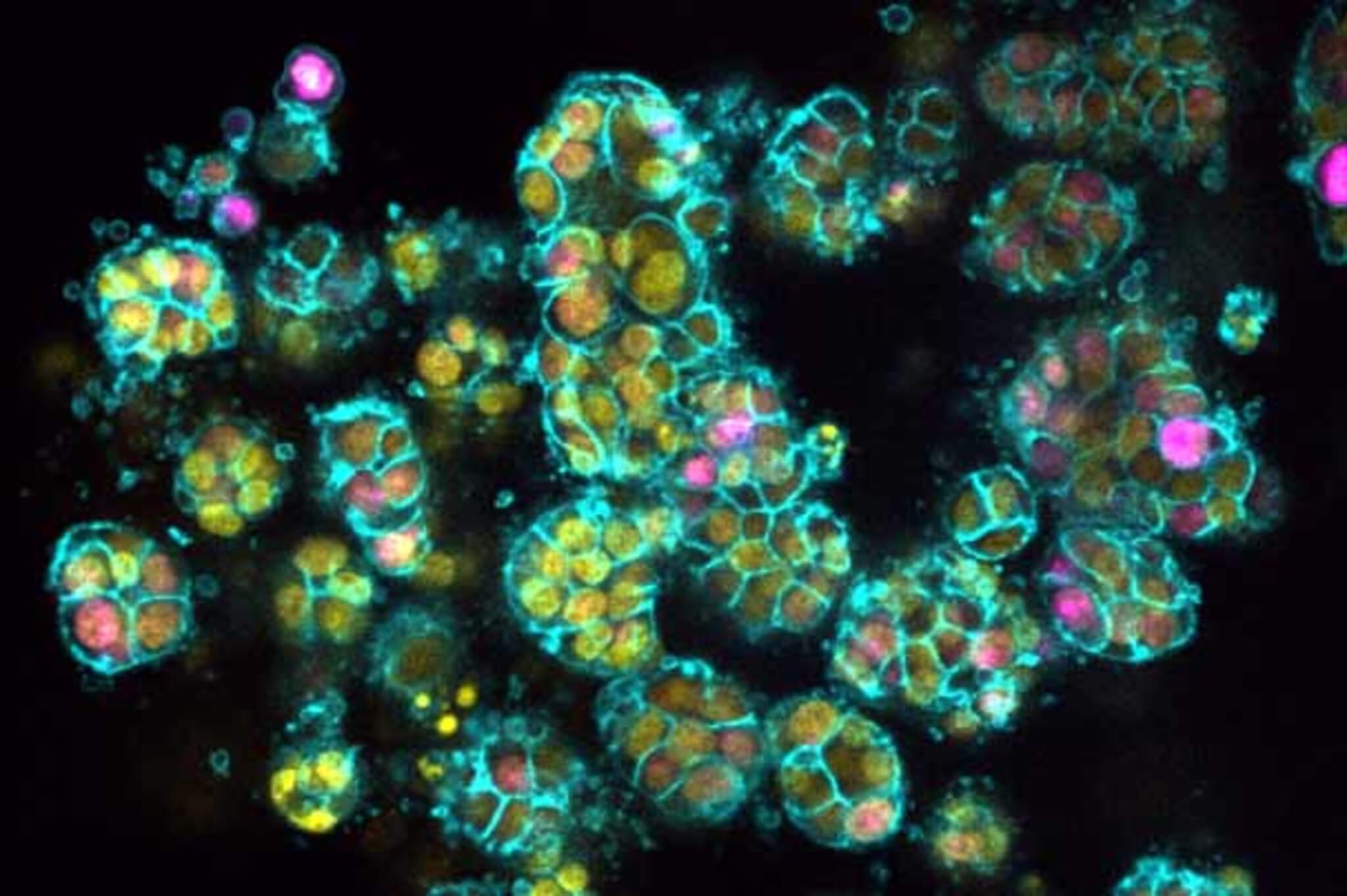
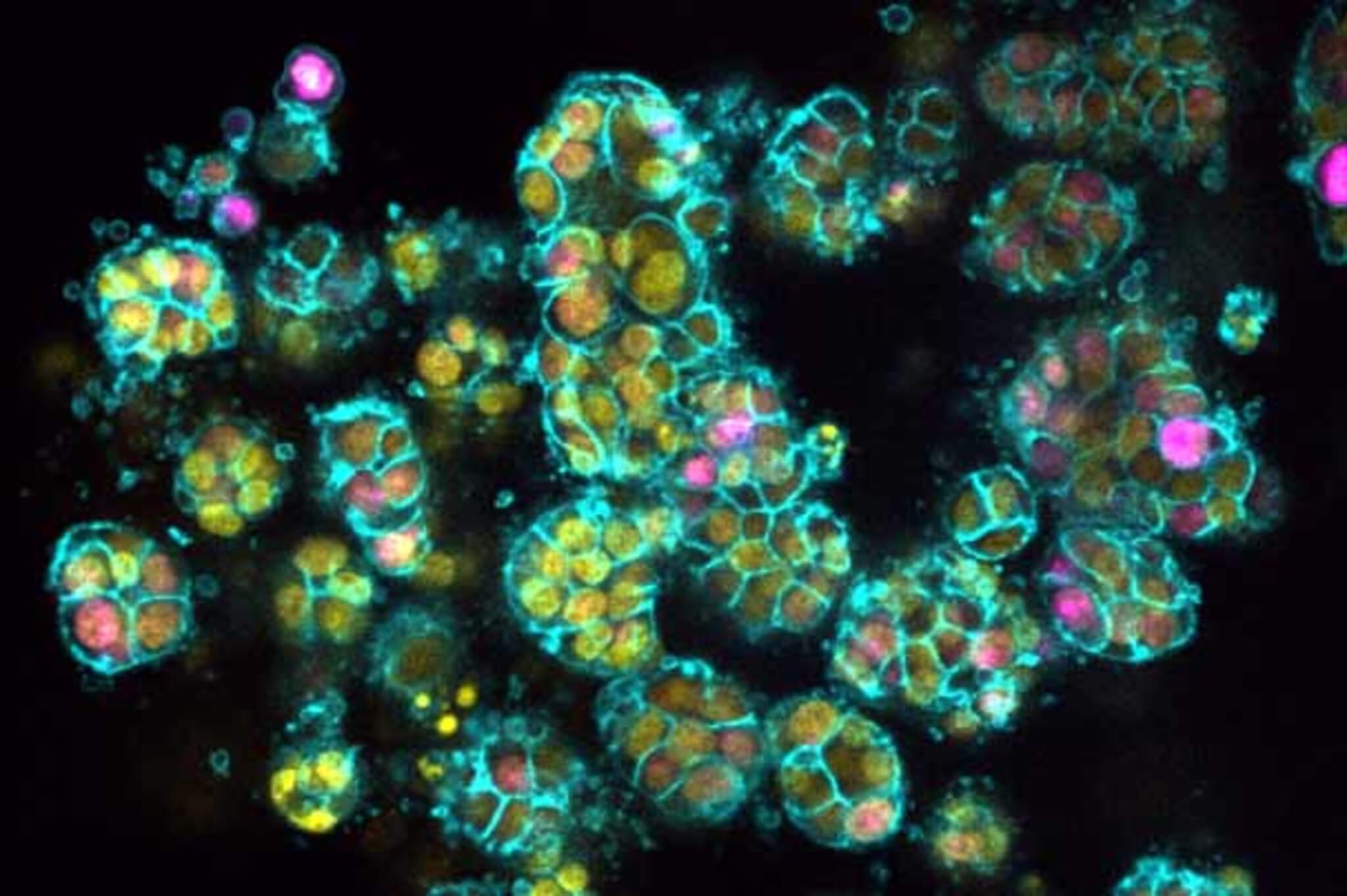
T cells are like the special forces of the immune system, trained to seek and destroy cancer cells. However, the study found that SAA proteins can throw a wrench in their mission.
“Our findings show that liver cells — with their release of SAA proteins — effectively serve as an immune checkpoint regulating anti-cancer immunity, making them a promising therapeutic target,” explains Dr. Beatty.
The research built upon the team’s earlier work, showing how liver inflammation promotes the spread of pancreatic cancer to the liver and is linked to worse responses to immunotherapy. In the new study, they wanted to dig deeper into the mechanisms behind this.
Using mouse models of pancreatic cancer, scientists observed that mice with less T cell infiltration in their tumors — a red flag that the immune response against the cancer is faltering — tended to have more liver inflammation. These mice also had increased activity in an inflammatory signaling pathway called IL-6/JAK/STAT3, which researchers had previously flagged as trouble in their 2019 study on liver metastasis.
Next, they found that activating STAT3 in liver cells led to a decrease in immune cells called dendritic cells, which are crucial for T cells to mount their attack on tumors. When UPenn researchers disabled STAT3 in the liver cells, dendritic cell production and T cell activity surged. The once T cell-deficient tumors were now flooded with cancer-fighting reinforcements.
The key culprit behind this effect are SAA proteins. The team discovered that STAT3 activation in liver cells suppresses dendritic cells and T cells by triggering the production of SAA proteins, which latch onto receptors on immune cells. Getting rid of the SAA proteins had the same immune-boosting impact as knocking out STAT3. In mice with pancreatic tumors that were surgically removed, this led to longer survival times and higher cure rates.
To check if these results might apply to humans, too, researchers examined tissue samples from pancreatic cancer patients who had undergone surgery. The team got excited after discovering patients with lower SAA protein levels at the time of surgery turned out to have significantly better survival rates.
This ability to translate the mouse findings to human patients underscores the potential clinical importance of the study.
“The translational findings in human patients highlight the likely clinical relevance of our discoveries in the mice,” notes Dr. Beatty. “Now that we’ve shown how liver inflammation puts up a roadblock to immunotherapy, our next step is to see if the same pathway can be targeted to reverse inflammation in patients who already have liver metastasis.”
UPenn researchers are now gearing up for further studies to test agents that inhibit STAT3 and SAA proteins. The hope is that these could be given in combination with immunotherapy to help improve outcomes for cancer patients. By targeting liver inflammation, we may be able to give the immune system the boost it needs to effectively combat cancer — a promising new angle of attack in the ongoing war against this devastating disease.